How many people have been infected by SARS-CoV-2? How many deaths have occurred? Nobody really knows the exact figures. There is a consensus that data on the number of COVID-19 pandemic cases and deaths are far from being exact. Additionally, in most cases, what is available for most users in national and international databases, dashboards, and bulletins is only basic information about the daily and cumulative numbers of cases, recoveries and deaths. It is a fact that in most countries, the collection, processing and dissemination of information has not been commensurate with data required for better informing policy decisions regarding the COVID-19 pandemic. Even European countries, where data collection is much better organized, cannot be considered as a gold standard either. It is understandable that the number of cases is difficult to know, as asymptomatic cases represent an important part of the total (probably between 18% and 31% of all infections[i]). This is also true when testing is not systematic nor centralized and where there is no national data collection strategy paired with strict mandatory reporting.
Even in the United States, the type and quality of data collected and disseminated is rather inadequate. When reporting, states follow different standards and practices[ii]. What is presented above could explain the unprecedented situation we are facing now, where it is the media (New York Times) and universities (John Hopkins University) that have built databases widely used by the public. At the global level, the monitoring system of the WHO is based on national reports which are incomplete and affected by changes in the criteria used to define a case or a death. WHO mentions a recent trend in some countries toward ‘data reconciliation exercises’ that can remove an important number of cases and deaths[iii].
How are deaths counted?
Although mortality is considered as one of the best indicator of the health impacts of COVID-19[iv], the counting deaths caused by this pandemic has either not been done or has been inadequate and deaths have probably been undercounted. The main reason is lack of preparation in most countries for reporting a pandemic such as COVID-19. Moreover, countries do not use the same definition or protocol to determine, record and report COVID-19 deaths.[v] Among the probable deaths that are not well counted are those that occurred outside hospitals and health centers. In Italy, the United Kingdom and Spain, deaths that occurred outside hospitals are not counted, contrary to Belgium and France where they are counted (in France after April 7th)[vi]. The case of deficiencies in the recording of deaths in homes and older persons’ residences, such as nursing homes, is notorious[vii]. In many cases, these deaths have not been reported, especially those that occurred at the start of the pandemic.
This situation worsened because of the lack in many countries of adequate epidemiological surveillance systems, and in some cases, the political interference that affects what is disclosed or limits the possibility of agreements on data collection, processing and reporting methods. In spite of recent developments in the ecosystem of data science, including big data and AI, the apparently simple activity of counting deaths has been plagued with uncertainties.
But even within the same country, parameters have changed during the process. The most common change was to include not only the confirmed deaths (of patients who tested positive for COVID-19) but also the probable deaths (of persons who died and had all the symptoms but were not tested). In the United States[viii], 23 of 50 states report only confirmed deaths, while 27 report both confirmed and probable deaths (22 provide separate data and 5 combine both). There are countless places where definitions have changed to include probable deaths. This is the case in New York City where the change was just implemented on April 7th to include a large number of deaths due to COVID-19 that were occurring at home and were not being counted[ix]. On April 17th, China increased the number of its COVID-19 death toll by 50 % to include probable deaths occurring at home that were not correctly counted by hospitals[x].
These decisions have not necessarily been bad, since it means that previously excluded COVID-19 deaths are now being included. However, frequent changes in how COVID-19 deaths are counted undermine public credibility. Furthermore, the use of different standards affects the comparability of data.
But the biggest limitation for calculating the effect on mortality is the scarcity of information on deaths due to COVID-19 classified by age for each sex. Quite simply, this information, vital to measuring the impact of COVID on mortality, is not systematically available in most cases. Even in cases where deaths are classified by age, they are not necessarily presented for each sex separately. Worse still is the case of countries whose data by age and sex are not processed, and if processed, are not disseminated. What is more unusual in this situation is that in many cases this is happening not only in least developed countries but also in some middle income and even some developed countries that generally have statistical systems that usually allow for faster access to quality data.
What this pandemic has clearly shown is a widespread lack of standardized systems for systematically and efficiently managing basic statistical data that need to be collected and widely disseminated in a pandemic situation. Among the efforts worth mentioning are those of the French National Institute for Demographic Studies (INED), which has created a database of deaths by sex and age standardized for the countries of Europe.
In countries with good vital statistical systems that count all deaths and identify the cause of death, better information will be forthcoming when the final data become ready and available, in most cases at the beginning of next year. But this is not the case in developing countries where systems systematically underreport deaths. This lack of good quality data on vital statistics also makes impossible the use of another strategy being used to determine the actual number of COVID-19 related deaths: the calculation of excess deaths and excess mortality due to COVID-19. This indirect demographic technique is being increasingly applied to calculate the number of COVID-19 deaths by comparing the number of expected deaths, based on information for previous year(s), with the actual number of deaths that occurred in 2020, which includes COVID-19 and non-COVID-19 deaths. This methodology allows for the estimation of the total number of both direct and indirect deaths[xi] caused by COVID-19 (See Figure 1 with the estimates for New York City[xii]). Unfortunately, developing countries with unreliable vital statistical systems are excluded from the possibility of applying this technique.
Figure 1: Number of confirmed and probableCOVID-19–associated deaths and total estimated excess deaths, New York City, March 11–May 2, 2020
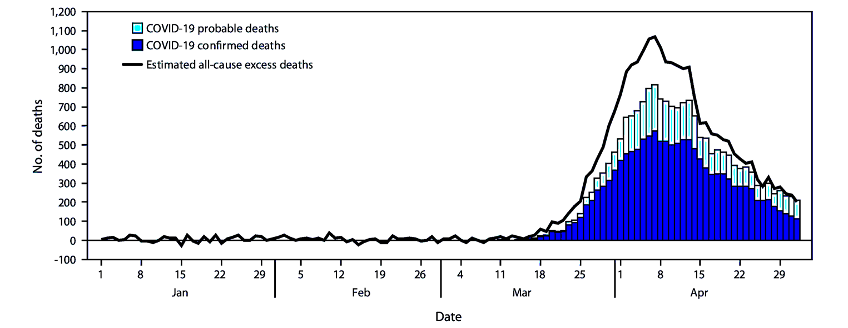
Source: Preliminary Estimate of Excess Mortality During the COVID-19 Outbreak — New York City, March 11–May 2, 2020. MMWR Morb Mortal Wkly Rep 2020;69:603–605. DOI: http://dx.doi.org/10.15585/mmwr.mm6919e5external
Final remarks
Agreements are needed between countries to define a more standardized way to count deaths, build databases including other key information such as age, sex, race, economic status and disseminate this information widely. Better definitions and agreements are required to deal with data uncertainties in the future. In the current era, there are no excuses not to do a better job in measuring well the impact on morbidity and mortality of the largest pandemic of the last century.
REFERENCES
[i] Seyed M. Moghadas, Meagan C. Fitzpatrick, Pratha Sah, Abhishek Pandey, Affan Shoukat, Burton H. Singer, and Alison P. Galvani. The implications of silent transmission for the control of COVID-19 outbreaks. PNAS first published July 6, 2020 https://doi.org/10.1073/pnas.2008373117
[ii] Tracking COVID-19 in the United States: From Information Catastrophe to Empowered Communities. https://preventepidemics.org/wp-content/uploads/2020/07/Tracking-COVID-19-in-the-United-States-Report.pdf
[iii] WHO (2020), Coronavirus disease (COVID-19). Situation Report – 181. Data as received by WHO from national authorities by 10:00 CEST, 19 July 2020.
[iv] García-Basteiro AL, Chaccour C, Guinovart C, et al. Monitoring the COVID-19 epidemic in the context of widespread local transmission. The Lancet Respiratory Medicine 2020; DOI:10.1016/S2213-2600(20)30162-4.
[v] Simone Ghislandi, Raya Muttarak, Markus Sauerberg, Benedetta Scotti. News from the front: Estimation of excess mortality and life expectancy in the major epicenters of the COVID-19 pandemic in Italy. International Institute for Applied Systems Analysis, Schlossplatz 1, A-2361 Laxenburg, Austria.
[vi] See Gislandi et al (ibidem).
[vii] In May, 2020, it was estimated that one-Third of All U.S. Coronavirus Deaths Are Nursing Home Residents or Workers. By Karen Yourish, K.K. Rebecca Lai, Danielle Ivory and Mitch Smith. Updated May 11, 2020. https://www.nytimes.com/interactive/2020/05/09/us/coronavirus-cases-nursing-homes-us.html . More recent data shows however that more than 40% of COVID-19 deaths in the United States have occurred in long-term care facilities including nursing homes. But the report by States shows inconsistencies: some reported deaths of both residents and staff working at these facilities. Not all include all the facilities either (See: Tracking COVID-19 in the United States: From Information Catastrophe to Empowered Communities. https://preventepidemics.org/wp-content/uploads/2020/07/Tracking-COVID-19-in-the-United-States-Report.pdf
[viii] https://www.nytimes.com/interactive/2020/06/19/us/us-coronavirus-covid-death-toll.html
[ix] https://gothamist.com/news/death-count-expected-soar-nyc-says-it-will-begin-reporting-suspected-covid-deaths-addition-confirmed-ones
[x] https://www.nytimes.com/2020/04/17/world/asia/china-wuhan-coronavirus-death-toll.html
[xi] Indirect deaths are those that occurs because of the lack of access to health services by people affected by non-COVID-19 illnesses, due to the disruptions resulting from the CVID-19 pandemic.
[xii] Preliminary Estimate of Excess Mortality During the COVID-19 Outbreak — New York City, March 11–May 2, 2020. MMWR Morb Mortal Wkly Rep 2020;69:603–605. DOI: http://dx.doi.org/10.15585/mmwr.mm6919e5external

This is a very helpful article and shows the problems confronting policymakers and the public as we all try to understand and manage the ongoing pandemic.
You are absolutely right. Thanks for your comment.